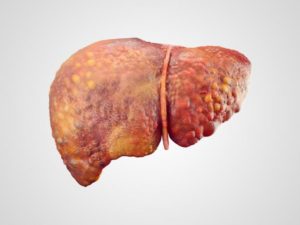
 Liver cancer, also known as hepatic cancer, is a cancer which starts in the liver, rather than migrating to the liver from another organ or section of the body. In other words, it is a primary liver cancer.
Liver cancer, also known as hepatic cancer, is a cancer which starts in the liver, rather than migrating to the liver from another organ or section of the body. In other words, it is a primary liver cancer.
Cancers that originate elsewhere and eventually reach the liver are known as liver metastasis or secondary liver cancers, and are most commonly from cancer of the gastrointestinal (GI) tract (colon cancer), lung cancer, renal cancer (cancer of the kidney), ovarian cancer and prostate cancer.
The liver, which is located below the right lung and under the ribcage is one of the largest organs of the human body. It is divided into the right and left lobes. Nutrient-rich blood is carried by the portal vein from the intestines to the liver, while oxygen-rich blood reaches the liver from the hepatic artery.
All vertebrates (animals with a spinal column) have a liver, as do some other animals. The liver has a range of functions, including detoxification (getting rid of toxins), synthesizing proteins, breaking down fats, and producing biochemicals that are essential for digestion. We cannot survive without a liver.
Symptoms and causes of liver cancer
Diagnosis, treatment and prevention of liver cancer
Fast facts on liver cancer
Here are some key points about liver cancer. More detail and supporting information is in the main article.
- The liver is a large and vital organ in all mammals
- Hepatocellular carcinoma is the most common type of liver cancer
- Liver cancer effects around 30 people per 100,000
- One of the major risk factors is excess alcohol intake
- Symptoms generally do not appear until the cancer is advanced
- Diabetes and hepatitis are risk factors for liver cancer
- Diagnosis can be made in a number of ways, including biopsy and blood tests
- Treatment options for liver cancer include surgery and liver transplant
- Cutting down alcohol intake can help reduce the chances of liver cancer.
What is liver cancer?
Liver cancer consists of malignant hepatic tumors (growths) in or on the liver.
The most common type of liver cancer is hepatocellular carcinoma (or hepatoma, or HCC), and it tends to affect males more than females. According to the National Health Service (NHS), UK, approximately 1,500 people in the United Kingdom die from HCC each year.
The World Health Organization (WHO) estimate that liver cancer’s prevalence is around 30 cases per 100,000 people worldwide, with rates in parts of Africa and Eastern Asia being particularly high.
Experts say that common causes of HCC are regular high alcohol consumption, having unprotected sex and injecting drugs with shared needles
Symptoms of liver cancer
Signs and symptoms of liver cancer tend not to be felt or noticed until the cancer is well advanced.
HCC signs and symptoms may include:
- Jaundice – skin, tongue and whites of the eyes become yellow
- Abdominal pain – often on the right side, may reach as high up as the shoulder
- Unexplained weight loss
- Hepatomegaly – enlarged liver, the abdomen may appear swollen
- Fatigue
- Nausea
- Emesis (vomiting)
- Back pain
- General itching
- Fever.
Causes of liver cancer
Anabolic steroids – used by athletes and weight lifters. These male hormones, if used regularly and for long enough, can raise the risk of developing liver cancer, as well as some other cancers.
Aflatoxins – a substance made by a fungus and may be found in moldy wheat, groundnuts, corn, nuts, soybeans and peanuts. For liver cancer risk to increase there needs to be long-term exposure. This is more of a problem in less wealthy countries.
Cirrhosis – when liver cells are damaged and replaced with scar tissue. People with cirr hosis of the liver have a higher risk of developing liver cancer.
hosis of the liver have a higher risk of developing liver cancer.
Diabetes – patients with diabetes, especially if they also have hepatitis, or regularly consume a lot of alcohol, are more likely to develop liver cancer.
Family history – people whose mother, father, brother, or sister had liver cancer are at a higher risk of developing it themselves, compared to others.
L-carnitine deficiency – studies suggest that an L-carnitine deficiency increases the risk of developing liver cancer.
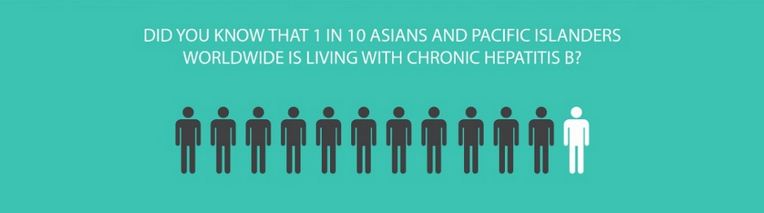
Liver disease and inherited liver disease – people with hepatitis B or C have a significantly higher risk of developing liver cancer, compared to other healthy individuals. According to the American Cancer Society, hepatitis C is the most common cause of liver cancer in the USA. The Society mentions that some inherited liver diseases also increase the risk of liver cancer.
Low immunity – people with weakened immune systems, such as those with HIV/AIDS have a risk of liver cancer that is five times greater than other healthy individuals.
Obesity – obesity raises the risk of developing many cancers, including liver cancer.
Gender – a higher percentage of males get liver cancer compared to females. Some experts believe this is not due to gender, but to lifestyle characteristics. On average, males tend to smoke and abuse alcohol more than females.
Smoking – individuals with hepatitis B or C have a higher risk of liver cancer if they smoke.
Water wells with arsenic – people who rely on water wells that contain arsenic may eventually have a significantly higher risk of developing several conditions or diseases, including liver cancer.
Diagnosis of liver cancer
HCC screening – high risk individuals for HCC should have regular screenings for liver cancer. Liver cancer, if not diagnosed early is much more difficult to remove. The only way to know whether you have liver cancer early on is through screening, because symptoms are either slight or nonexistent.
High risk people include those with hepatitis C and B, patients with alcohol-related cirrhosis, other alcohol abusers, and those that have cirrhosis as a result of Hemochromatosis.
Diagnostic tests for liver cancer include:
- Blood test – AFP (alpha fetoprotein), a type of protein, is produced by liver tumors and can be detected in a blood test
- Imaging scans – either an MR
 I or CT scan
I or CT scan - Biopsy – a small sample of tumor tissue is removed and analyzed. The analysis can reveal whether the tumor is cancerous (malignant) or non-cancerous (benign).
Liver cancer is categorized into four stages:
- Stage 1 – the tumor is just in/on the liver and nowhere else
- Stage 2 – either there are several small tumors, but all within the liver, or one tumor that has reached a blood vessel
- Stage 3 – either there are various large tumors, or there is just one that has reached the main blood vessel(s). Cancer may have also reached the gallbladder
- Stage 4 – metastasis. The liver cancer has spread to other parts of the body.
Treatment options for liver cancer
Unfortunately, because symptoms do not appear until the liver cancer is well advanced, currently only a small percentage of patients with HCC can be cured; according to the NHS only about 5% can be saved.
Liver cancer treatment options include:
Treating curable cancer
- Surgery – in the early stages, when the tumor is small and occupies just a small part of the liver, it can be surgically removed (surgical resection). Even if part of the liver is removed during this procedure, the patient’s health should not be significantly undermined
- Liver transplant – candidates for a liver transplant cannot have a tumor larger than 2 inches (5cm), according to the NHS. If the tumor is larger, the risk of the cancer coming back is too high, says the NHS.
Treating non-curable cancer
If the liver cancer has had a chance to advance, the likelihood of a cure is extremely small. However, there are things the medical team can do to treat symptoms and slow its advancement.
- Ablative therapy – substances are injected directly into the tumor, such as alcohol. Lasers and radio waves can also be used
- Radiation therapy (radiotherapy) – radiation is directed at the tumor(s), killing a significant number of them. Patients may experience nausea, vomiting and fatigue
- Chemotherapy – medications are injected into the liver to kill cancer cells (chemoembolization). In chemoembolization the blood supply to the tumor is blocked surgically or mechanically and anticancer drugs (chemotherapy) are administered directly into the tumor
- Volunteer for clinical studies – when trials reach the human stage they are called clinical trials. Ask your doctor whether there are any available in which you may be able to take part.
Treatment options may vary, depending on the type of liver cancer. For cholangiocarcinoma the medical team may recommend photodynamic therapy, brachytherapy, radiotherapy or liver transplantation. For hepatoblastomas, doctors may use chemotherapy, radiation therapy, liver transplantation, or surgical resection.
How can liver cancer be prevented?
Alcohol: long-term, regular high alcohol intake significantly increases the risk of cirrhosis of the liver, which in turn makes the likelihood of developing liver cancer much greater. It stands to reason, therefore, that moderating one’s alcohol intake (or giving up completely) can significantly reduce the risk of developing liver cancer.
Hepatitis B: The following individuals should seriously consider receiving the hepatitis vaccine: drug addicts who share needles, individuals who engage in unprotected sex with partners who may be at risk of having hepatitis B, nurses, doctors, dentists and other individuals whose occupations raise their risk of becoming infected. Frequent travelers, especially those who go to parts of the world where hepatitis B is common should also consider being vaccinated.
Hepatitis C: Although there is no sure way of protecting oneself from hepatitis C, using a condom during sex may help reduce the risk of infection. There is no hepatitis C vaccination (July 2010).
 Female Cancer Specialist Doctor in Kanpur female, doctor, cancer, specialist, female, oncologist, oncology, medical, oncologist, chemotherapy, breast, blood, mammography, prostate, center, hospital, radiotherapy, surgery, mouth, kanpur, sn, memorial, female, doctor, cancer, specialist,
Female Cancer Specialist Doctor in Kanpur female, doctor, cancer, specialist, female, oncologist, oncology, medical, oncologist, chemotherapy, breast, blood, mammography, prostate, center, hospital, radiotherapy, surgery, mouth, kanpur, sn, memorial, female, doctor, cancer, specialist,